Management: Lymphatic Malformations and Lymphedema
How Does the Lymphatic System Work?
To understand lymphatic malformations and lymphedema, let's look at the lymphatic system.
The lymphatic system is a part of the circulatory system, and a vital part of the immune system.
Arterial blood carries oxygen, nutrients, and hormones for the cells. To reach these cells the blood leaves the small arteries and flows into the tissues. This fluid is now known as interstitial fluid and it delivers its nourishing products to the cells. Then it leaves the cell and removes waste products.
After this task is complete, 80-90% of this fluid returns to the circulatory system as venous blood.
What Is Lymph?
The remaining 10-20% of the fluid that stays behind in the tissues is a clear to yellowish fluid known as lymph.
Lymph is formed when the fluid that lies in the spaces between body tissues (interstitial fluid) is collected through lymph capillaries. It is then transported through lymph vessels to lymph nodes before emptying ultimately into the right or the left subclavian vein, where it mixes back with blood.
The word lymph is derived from the name of the Roman deity of fresh water, Lympha. (Wikipedia)
Unlike blood, which flows throughout the body in a continuous loop, lymph flows in only one direction within its own system - upward toward the neck. This upward movement from the interstitial spaces up through the body depends on the motion of muscle and joint pumps, temperature, diaphragmatic breathing and pulsation in adjacent arteries.
As it makes its way through the body, lymph passes through lymph nodes that filter out debris and pathogens. The tonsils, adenoids, spleen and thymus are all part of the lymphatic system. When the filtered lymph reaches the neck, it flows into the venous blood stream through the subclavian veins, located on either side of the neck near the collarbones.
Since the lymph is derived from interstitial fluid, its composition continually changes as the blood and the surrounding cells constantly exchange substances with the interstitial fluid. It is generally similar to blood plasma except that it also contains white blood cells. Lymph returns proteins and excess interstitial fluid to the bloodstream. Lymph may pick up bacteria and bring them to lymph nodes where they are destroyed. Metastatic cancer cells can also be transported via lymph. Lymph also transports fats from the digestive system. (Wikipedia)
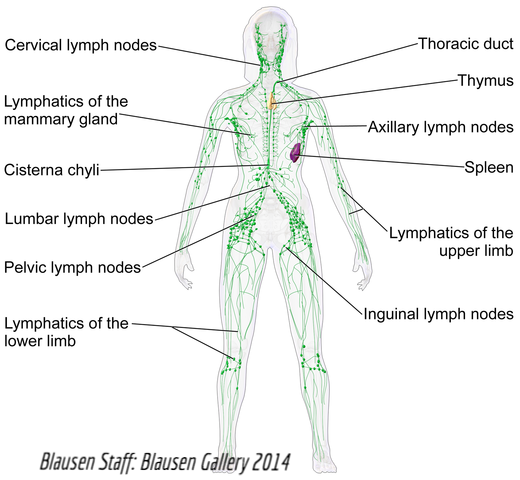
The Lymphatic System
Lymphatic Malformations
Lymphatic malformations are fluid filled channels or vessels where the lymphatic system has not developed properly, causing dilated vessels and clear fluid accumulation as a result of the slow flowing lymph.

Blood filled blebs
Lymphatic malformations (LM) tend to grow between the skin and muscle. There may also be asymmetry, distortion and bone overgrowth. LM in an extremity is frequently associated with lymphedema. When they occur closer to the skin, they may manifest as vesicles or blebs that are clear or bluish, or Capillary bleeding can mix with the lymph fluid, causing the blebs to appear filled with blood (see photo).
Lymphatic malformations can have tiny fluid spaces (microcystic) or large fluid spaces (macrocystic), or they can be a combination of both. They can be in only one area, or very extensive, affecting multiple parts of the body. Proper diagnosis is important as treatment for each type is different. Your physician might recommend compression garments to control filling of dilated lymphatic channels and swelling of extremities. Keeping the area of the lymphatic malformation clean is also extremely important as it reduces the risk of skin breakdown and infection, particularly for lesions involving the feet and legs. Risk of infection is always present.
Sudden enlargement of a lymphatic malformation is likely the result of bleeding or an infection (cellulitis). If there is an infection involving an area that contains a lymphatic malformation, antibiotic therapy must be initiated. Cellulitis can be differentiated from bleeding most often by symptoms of redness and heat over the lymphatic malformation. Since some strains of bacteria can be dangerous, if you suspect cellulitis you should seek medical attention as soon as possible. Bleeding into a lymphatic malformation can be painful and should also be seen by a physician.
Children's Hospital of Cincinnati
Children's Hospital of Los Angeles
Lymphedema
The lymphatic system is made up of vascular channels that are only visible on certain scans. Lymph is that protein rich fluid that helps carry certain fats and white blood cells (lymphocytes) through the body and also help carry away cell impurities. When excess lymph fluid leaks our of the lymphatic vessels into the surrounding tissue, the condition is called lymphedema.
Lymphedema is characterized by excessive fluid retention and swelling of the affected area due to abnormalities or poor functioning of the lymphatic system.
- The affected area may be larger than other body areas, have an "obese" look, and appear lumpy or uneven.
- There may also be symptoms such as lymph fluid weeping through the skin, fluid filled bumps or "blebs", as well as a feeling of heaviness and/or pain in the affected area.
- Ascites (lymph filled cavities in the abdominal or pelvic region) may show up on scans.
There are two key types of lymphedema:
- Primary lymphedema: This is caused by pre-existing abnormalities or "malformations" usually present at birth that cause poor function of the lymphatic system. There may be overgrowth of the lymphatic system in one or more areas, missing portions of the lymphatic system, or other abnormal structuring leading to symptoms.
- Secondary lymphedema: This is lymphedema that develops gradually across time as a result of impaired blood vascular flow. For example, someone with impaired venous function may initially develop a condition called "vascular edema", which is fluid retention and swelling caused by impaired blood flow but is not related to the lymphatic system. However, over time, this condition can cause stress to the lymphatic system, causing it to function poorly. At this point the person will develop lymphedema that is secondary to (or indirectly caused by) impaired vascular flow.
(Laredo J & Lee NN. Lymphedema-Chapter 23 of Phlebology, vein surgery, and ultrasonography. 2014 ed.) (Liu, Lu, Yan, 2010. J.Vasc Surg) (Fialka-Moser et al. 2013J. Rehab)
In cases of vascular anomalies, lymphedema can be isolated or it can accompany other symptoms. It can affect one area of the body, or several. It can be due to a developmental issue in the lymphatic vascular development (primary), a result of obstructed of lymphatic flow (secondary), or both. Anyone treating lymphedema in a combined vascular malformation should have knowledge of lymphatic malformations.
The lymphatic system is a part of the vascular system. In K-T and similar phenotypes, lymphatic malformations are one of the components making up the diagnosis. Lymphatic malformations are different from lymphedema.
Living with Lymphedema
Responsibility for management of lymphedema falls on the patient in most cases. Self education about the condition and how to manage it are a critical part of managing overall health. Management involves decongesting the reduced lymphatic pathways; encouraging the development of collateral drainage routes and stimulating the function of remaining patent routes.
Steps you can take to avoid problems in areas prone to lymphedema:
- Find a good source for education material.
- Find a certified lymphedema therapist early. There is no U.S. government recognized standard for training, but we recommend therapists who follow guidelines established by the Lymphology Association of North America (LANA), which includes a minimum of 135 hours of training to be considered qualified.
- Elevate the affected extremity whenever possible.
- Use compression as advised by physician.
- Avoid applying heat to the affected area.
- Risk of infection is elevated, and can result from bacteria or fungus entering minute cracks or dry areas of the skin. Skin infections are known as cellulitis (or erysipelas) and can be very serious, even life threatening. Keep your skin and nails clean to avoid infection.
- Learn to recognize inflammation, cellulitis, and lymphangitis, and when to seek medical attention.
- Protect yourself from injury, especially to the limb(s) most likely to be affected.
- Do not wear tight clothing.
- Avoid positions, movements, or activities that may constrict your circulation (carrying heavy bags, crossing legs, tight socks or jewelry).
- Habitually practice some sort of exercise (walking, swimming, biking, yoga).
- Avoid bare feet.
- Take precautions during periods of prolonged immobilization and when traveling.
- Let your lymphedema therapist know if you are taking anticoagulants, especially prior to CDT.
- Avoid blood draws, immunizations (includes other needles) or blood pressure measurement in the area that has lymphedema.
- Talk with your physician about the need to have on hand a prescription for an antibiotic should there be an episode while traveling.
Stages of Lymphedema
Stage 0 - Pre-Stage: Latency or Subclinical Stage
There might be no visible changes outwardly, or there might be progressive swelling or fullness in a limb, or one might experience tingling, a tiredness or heaviness or even pain in the affected area.
Lymphedema can remain in the latency stage for months or even years before symptoms become obvious.
Stage I - Pitting Edema
If the latency stage is ignored or missed, pitting edema may occur. This is the first stage of lymphedema, also called reversible lymphedema. The affected area will become mildly swollen, filled with protein rich lymph fluid (versus venous edema). Pressing into the tissue will often cause a small dent or "pit" to appear. Symptoms resolve with elevation but usually worsen during the day. With elevation or bedrest, the limb should return to normal. At this stage there is no skin or tissue damage resulting from the lymphedema.
Stage II - Spontaneously Irreversible Lymphedema
Tissue changes (inflammation, hardening, thickening) are happening. Progression of swelling occurs. Skin hardens and the swelling no longer resolves upon waking. Pitting is less because of the tissue fibrosis. Stage II lymphedema will respond to treatment but tissue damage cannot be reversed.
Stage III - Lymphostatic Elephantiasis
Pitting no longer occurs. At this point the disease has progressed to include permanent trophic skin changes (changes resulting from interruption of nerve supply). Skin is dry and scaly, and there might be fluid leaking from the limb. Skin infections are common. The affected area of the body becomes very large and misshapen. The skin will have warty overgrowth, appearing leathery and wrinkled, and some skin projections or blisters might appear, attempting to contain the fluid.
Traditional treatment of lymphedema
(Finnane et al. 2015)
There is no accepted cure for lymphedema at this time. Therefore treatments must be repeated periodically to keep the condition manageable. Traditional treatments are listed. A combination of treatments is termed Complete Decongestive Therapy. (CDT). CDT consists of an initial reductive phase followed by a maintenance phase. The main goals of early CDT are reducing the size of the affected part and improving the skin. Effects of CDT are
- decrease swelling
- increase lymph drainage from the congested area
- reduce skin fibrosis and improve skin condition
- enhance patient's functional status
- relieve discomfort and improve quality of life
- reduce the risk of cellulitis and Stewart-Treves Syndrome, a rare form of angiosarcoma
Components of CDT are:
- Manual lymph drainage (MLD): This method may involve wrapping the affected area with bandaging, using MLD massage techniques, or a combination of these. A licensed MLD therapist, preferably a certified lymphedema therapist, but often a physical or occupational therapist) should initiate the treatment. Once goals are achieved, the patient will be released from therapy with a home maintenance plan.
- Compression therapy (short stretch bandages and compression garments)
- short stretch bandages are used during the intensive phase of CDT as the volume of the limb changes almost daily, thus whole garments would have to be constantly refitted
- Compression garments are typically worn for maintenance so as to limit additional swelling, or recurrence of swelling.
- Lymphatic exercise
- Skin care and education
Lymphedema garments come in a variety of styles and degrees of compression. The type of garment, compression gradient, and whether the garment is off-the-shelf or custom measured can depend on patient needs.
Some types of inelastic leggings, the Unna boot and pneumatic compression are sometimes used short-term treatments, like ulcerations. Other inelastic types, like Solaris or Tribute, are known to be comfortable and effective but are primarily designed to wear at home.
Traditional elastic garments are currently the most well-known option, and used for daily treatment. The chart below lists a variety of garments, both custom and off the shelf.
| Compression Company | Type of Product | Custom/Off-the-Shelf |
|---|---|---|
| Solaris | Night garments,Ready Wrap, stocking/sleeve, Swell Spots | Custom, Off-the-Shelf |
| Barton Carey | Stocking/Sleeve | Custom |
| Bio-Concepts | Stocking/Sleeve | Custom, Off-the-Shelf |
| Juzo | Stocking/Sleeve | Custom, Off-the-Shelf |
| Jobst | Stocking/Sleeve | Custom, Off-the-Shelf |
| Mediven | Circaid, Stocking/Sleeve Circaid Juxtafit (inelastic) | Custom, Off-the-Shelf |
| Lymphadiva | Sleeve | Off-the-Shelf |
| Sigvaris | Stocking/Sleeve | Off-the-Shelf |
Pneumatic lymphedema pumps: Although not a part of traditional CDT, pneumatic lymphedema pumps are effective at both reduction of swelling and maintenance to prevent future swelling. Lymphedema pumps must be used regularly to be effective in keeping lymphedema under control. These devices use gradient pressure, meaning they pump upward to push the lymph fluid our of the affected area so the body can excrete the excess fluid.
Elevation helps with allowing the lymph fluid to drain toward the lymph node areas and into the thoracic duct, while skin care such as moisturizing reduces risk of infection and ulcerations.
Elevation and Skin Care
Various forms of exercise including physical therapy exercises, lymphedema specific exercises, sport related activities, and even yoga have been shown to reduce lymphedema and improve outcomes. (Morris & Wonders, 2015) (Ahmed et al. 2006) (McNeely et al. 2010) (Aggithaya et al. 2015) Although much of the findings reference cancer-related lymphedema, the usefulness of exercise still applies to those with lymphatic malformations, including those with K-T and other combined vascular malformations. The reason exercise works is that the combination of motion and muscular influence help to "pump" the lymphatic fluid through the vessels and out into the blood stream.
Complications in Lymphedema
- Lymphangiectasia (Ingle and Ingle, 2014) (Wen et al. 2010) The prevalence of this condition in K-T and other lymphatic malformation disorders is unknown, however the potential for it to develop is present. Lympangiectasia is a form of "protein losing enteropathy". Essentially lymph fluid leaks into the gut or renal system causing protein loss and malabsorption of nutrients (Kumar et al. 2014). Symptoms may include frequent diarrhea, nausea, protein deficiency (low blood albumin or prealbumin), vitamin deficiencies, ascites present on scans, and intolerance to high fat foods. Treatment is dietary and typically consists of a high-protein low-fat diet, with nutritional supplements as clinically recommended. One study does indicate medium chain triglycerides could be therapeutic, (Desai et al. 2009). Also, there is a single case study of the drug Everolimus successfully treating pediatric intestinal lymphangiectasia (Ozeki et al. 2016. Pediatrics) Lymphatic scanning typically is diagnostic, although other methods have been used in the past for diagnosis.
- Lymphadenitis: This is inflammation of the lymph nodes.
- Infection: The pooling of lymph fluid, effects on immune function, and potential skin breakdown, in lymphedema dramatically increases the risk of infections. This includes cellulitis and infections of the lymph nodes and lymphatic vessels themselves(1)(2), lymphangititis, erysipelas, and sepsis. 1) (Carlson. 2014.ClinDermatol) 2)(Vaillant & Gironet, 2002)
- Lymphangiosarcoma: a rare complication of chronic lymphedema, sometimes referred to as Stewart-Treves Syndrome (Komoroswski AL, Wysocki WM, Mitus J. Angiosarcoma in a chronically lymphedematious leg: an unusual presentation of Stewart-Treves syndrome. South Med J. 2003; 96(8):807-8)
Imaging
Scans to map lymphatic malformations are frequently used not for diagnostic purpose (though that can sometimes be the case), but more often for confirmation of diagnosis or a clearer idea of how specifically the person's lymphatic system is affected. Methods for scanning lymphatic vasculature are listed. (Lohrmann, 2007. Br J Radiol) (Liu, Zhang. 2014 J Recons Microsurg)
- MRI Lymphangiography (MRL): The most current form of evaluating lymphatic system structure, using magnetic resonance imaging (MRI) technology combined with a compatible contrast.
- Lymphoscintography: Isotope contrast combined with computer aided tomography scanning
- Lymphography: Generally no longer performed. Iodine oil is used for contrast of lymphatic vessels while X-ray images are taken
Support for Lymphedema
Helpful support and more information is available at the National Lymphedema Network, or Lymphatic Education and Research Network.
Page last updated April 8, 2016